Does my child need antibiotics?
It’s that time of year again; coughs, colds, temperatures and the quandary of whether your child is OK to go to school. We forget each year just how disruptive this can be, how one infection seems to run into another and how our daily plans are put to one side to look after our unwell children. When children are brought to the doctor, be it in hospital, general practice or out of hours, it is because parents are worried. One frequent question we hear is whether they would benefit from an antibiotic. Thankfully this question has been extensively studied and there is strong evidence to guide us here.
Antibiotic resistance is a global public health threat, that already claims the lives of millions globally. Without antibiotics healthcare, and indeed society as we know it, would simply cease to function. Antibiotics are very commonly prescribed for children presenting with uncomplicated lower respiratory tract infections (LRTIs), however there is little evidence from randomised controlled trials (the strongest form of evidence we have) that antibiotics are effective. The below landmark trial we assessed whether amoxicillin reduced the duration of symptoms in children presenting with uncomplicated LRTIs in the primary care setting.
https://www.thelancet.com/article/S0140-6736(21)01431-8/fulltext
This double-blind, randomised, placebo-controlled trial was carried out in 56 general practices in England. 432 children were randomly assigned to the antibiotics group (n=221) or the placebo group (n=211). No differences were seen between the treatment. The authors found that amoxicillin for uncomplicated chest infections in children is unlikely to be clinically effective.
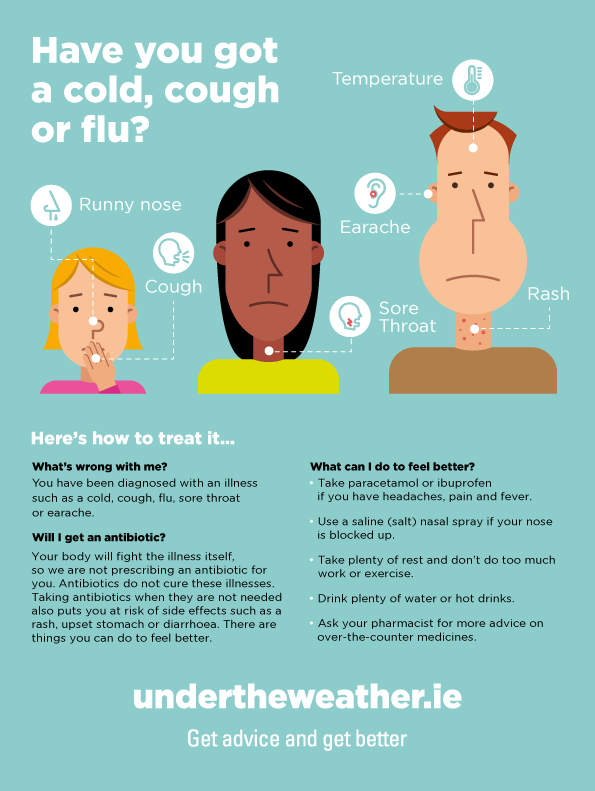
Ireland’s Expert Advisory Committee on antibiotics advise;
- Young children can develop 6-12 respiratory tract infections per year usually accompanied by cough
- In most children the cough can last 1-3 weeks.
- Acute cough in children is mainly caused by a self-limiting viral upper respiratory tract infection and resolves without antibiotics within 3-4 weeks.
- Associated symptoms include coryza (runny nose), sneezing, pyrexia (temperature).
- Antibiotics do not generally improve the overall clinical condition.
- Antibiotics are not indicated for acute cough in children, unless child is systemically very unwell or at high risk of complications.
Furthermore they advise;
- Ensure vaccinations are up to date.
- Avoid exposure to irritants such as cigarette smoke.
What to watch out for
If your child becomes irritable/drowsy/has decreased urine output/change in breathing/temp >39 degrees/rigors / otherwise systemically very unwell please call (or out of hours GP if outside of working hours)
Return if symptoms don’t improve after 3-4 weeks.
What can I use for symptom relief?
Honey can be used in children >1 year of age for a soothing effect (hot water with honey and lemon). There is poor evidence for other cough bottles.
Paracetamol and (if appropriate ibuprofen) are recommended for associated pain and temperatures.
You can consult your pharmacist for further symptom relief.
See below for links
https://www.hse.ie/eng/services/list/2/gp/antibiotic-prescribing/